Amplifying Cesarean Awareness
“The U.S. Cesarean rate continues to climb annually, and is currently at its highest rate, affecting 1 in 3 women and babies. Nature isn’t failing us one third of the time. The system is failing us.”
Cynthia Overgard, Pathways to Family Wellness, Issue 40.
In the United States just over 1 in 3 babies (1.3 million) are born each year surgically via cesarean. (1) See Consumer Reports’ national campaign here. Because women matter, we have to consider the circumstances in which women actually need such an invasive delivery method. This is, afterall, a major operation with serious risks of hemorrhage, infection and longer postpartum recovery time, to name a few. (2) Cesarean prevention efforts exist because c-sections, whether planned or unplanned, whether life-saving or elective, affect a woman’s overall health and future pregnancies. (3)
Data shows that individual hospital cesarean rates for first-time mothers with low risk deliveries varies widely. The variance means that not all care providers practice evidenced-based care. Many obstetricians choose to make the cut too often and for the wrong reasons. (4)
While the the Department of Health & Human Services set a national goal for c-section rates--- 23.9% (5) to try to help reduce the practice of unnecessary cesareans, it is still remarkably higher than the World Health Organization’s recommendation of between 10-15%.
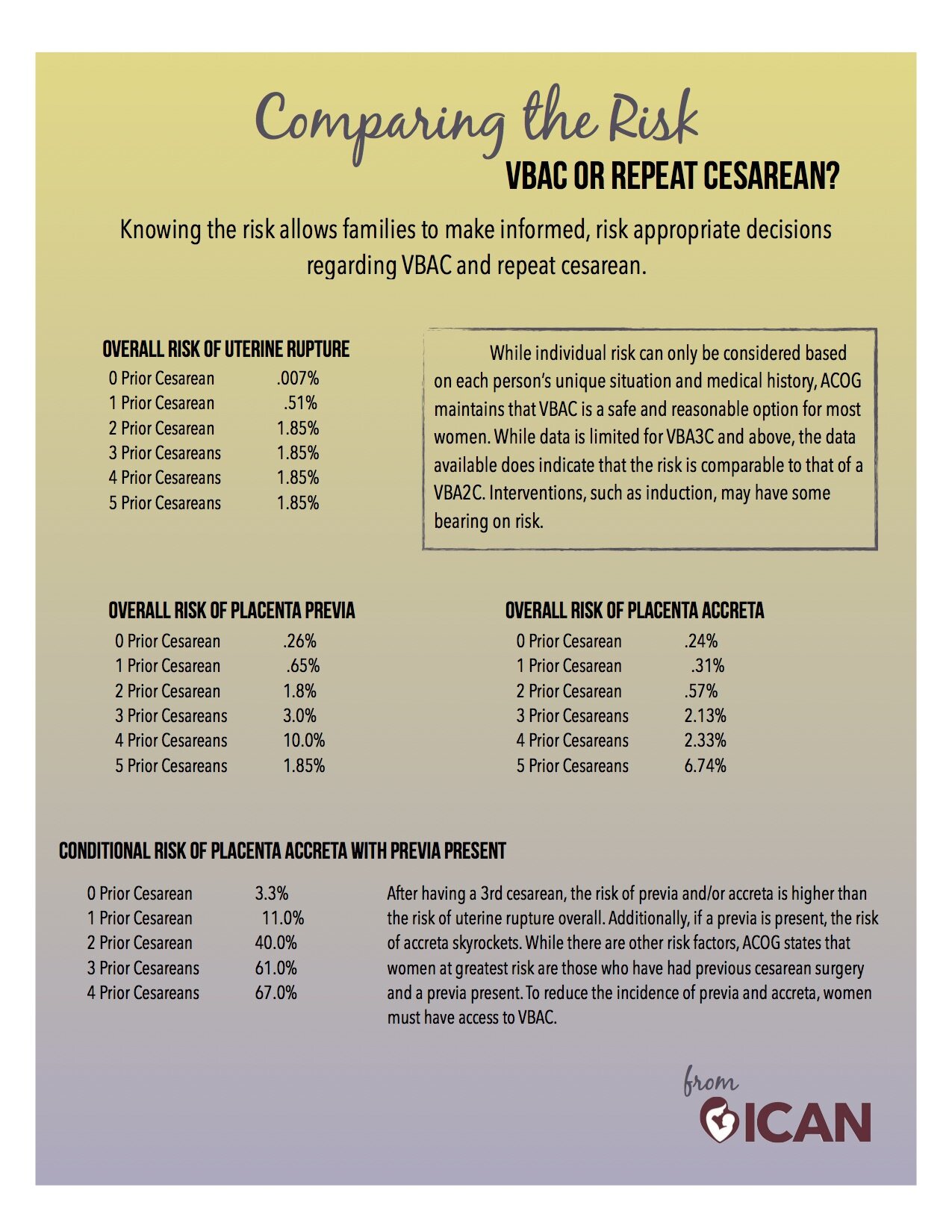
Also, there’s just a lot of incorrect information out there regarding what necessitates cesarean, repeat cesareans and VBAC (vaginal birth after cesarean). For example: ‘once a cesarean, always a cesarean’ is, in a word: false. And many women hear from their care providers that ‘repeat cesarean is safer than VBAC’. MYTH. Do yourselves a favor, and familiarize yourself with actual data.
ACOG (American College of Obstetrics and Gynecology) does acknowledge that primary cesareans affect future births, and planning vaginal delivery is safe and appropriate, when there is no maternal or fetal indications for cesarean delivery. It’s up to consumers to ask their care providers if they’ve implemented ACOG’s recommendations.
And, though many care providers do not support VBAC, the NIH (U.S. National Institutes of Health) reports: “Women who have a trial of labor, regardless of ultimate mode of delivery, are at decreased risk of maternal mortality compared to elective repeat cesarean delivery.” (6)
Cesareans should be reserved for situations of serious complications in mother and/or baby. Examples include, but are not limited to maternal medical conditions (severe hypertension, diabetes, heart disease, active herpes lesion), prolapsed cord, placenta previa, placental abruption, fetal malpresentation, serious hemorrhage, or when baby won’t come low enough in the birth canal for pushing or assisted delivery; or fetal distress (including respiratory distress); and other complications mentioned HERE.
When a mother consents to induction for non-emergent reason, or elects to have a cesarean for non-medical reasons, has her care provider provider made her aware of all the risks? Does she know she has choices? Mothers should be able to expect that their care provider will offer evidenced-based information, compassionate language about their birth and their expectations, and most of all, attentive, quality medical care. The brilliant Marsden Wagner offers some context for the right to choose cesarean here.
Further, a misconception of the ‘cesarean awareness’ effort is that all women should feel ashamed for having a cesarean, or at the very least feel scarred by it. That’s terrible. Mothers often have their feelings regarding cesarean birth dismissed. Example: “at least you have a healthy baby” or “you should be thankful that the surgery exists!” People don’t always know what to do with complex medical situations. It doesn’t help that certain phrases are associated with mothers in birth: arrested labor, trial of labor, failed vbac, etc. They don’t have the words because they don’t know that a woman may feel that her passage into motherhood was interrupted, that her body is broken, the physical process of going through labor and surgery caused a discombobulated postpartum recovery, or---- that she feels she ‘failed’ at birth.
When we limit our attitude about c-sections to ‘a surgery that can save the life of both the mother and the baby’, we essentially limit the compassion we have for a mother’s holistic health.
Women certainly don’t need to be told how to feel about their birth, and no one is forgetting the privilege it is to have access to quality emergency medical care. The truth is that some women need cesarean deliveries. Planned cesareans and unplanned cesareans need processing, just like any birth.
During her lecture on “The Case for Planning VBAC” at the International Cesarean Awareness Network 2016 Conference, Henci Goer charged the audience with this: “Don’t contribute to the conspiracy of silence”.
Supporting women in birth means vocalizing what mothers deserve: dignifying, humanizing care.
Whether you’re a friend, a father, or a birth worker, we have to be involved in amplifying this kind of care. Doulas can, at the very least, help women advocate for themselves by encouraging them to have expectations on their care provider. When the ‘system is failing us’ offering a steady voice of truth AND compassion will help a laboring mother root herself in the present and breathe through the passage of birth, however it uniquely unfolds.
The International Cesarean Awareness Network, Inc. (ICAN) is a nonprofit organization whose mission is to improve maternal-child health by preventing unnecessary cesareans through education, providing support for cesarean recovery, and promoting Vaginal Birth After Cesarean (VBAC). See local support groups here.
Read how to distinguish if a care provider is VBAC tolerant or VBAC friendly.)
For more information on evidence surrounding induction, c-sections and vbac facts visit Improving Birth .
Here is a great resource- 7 Tips for Cesarean.
Common myths associated with cesarean and vbac can be found here.
-------------------------------------------------
http://www.acog.org/Resources-And-Publications/Obstetric-Care-Consensus-Series/Safe-Prevention-of-the-Primary-Cesarean-Delivery#2
American College of Obstetricians and Gynecologists ( August 2010). Vaginal birth after previous cesarean delivery. Practice bulletin number 115. Retrieved from http://www.acog.org/Search?Keyword=Vginal+birth+after+previous+cesarean
Goer, H., Romano, A., & Sakala, C. (2012). Vaginal or cesarean birth: What Is at stake for mothers and babies? A best evidence review. New York: Chlldbirth Connection. Retrieved fromhttps://childbirthconnection.org/pdfs/vaginalorcesareanbirth.pdf
http://www.who.int/mediacentre/news/releases/2015/caesarean-sections/en/
Cunningham, FG, Bangdiwala S, Brown SS et al. (2010). National Institutes of Health Consensus Development Conference Statement: Vaginal birth after cesarean: New insights. March 8-10, 2010. Obstetrics & Gynecology, 115(6),1279-1295.
LOCAL CESAREAN RATES compiled by Ann Marie Walsh, of Second Heartbeat Education